Stacy Fritz, PT, PhD;1 Michelle Lusardi, PT, PhD2
1 Clinical Assistant Professor, Physical Therapy Program, De- partment of Exercise Science, Arnold School of Public Health, University of South Carolina, Columbia SC
2 Professor of Physical Therapy & Geriatrics, Dept. of Physical Therapy & Human Movement Science, College of Education & Health Professions, Sacred Heart University, Fairfield, CT
Walking speed is “almost the perfect measure.”1 A reliable, valid,2,3 sensitive4 and specific5 measure, self-selected walking speed (WS), also termed gait velocity, correlates with functional ability,6 and balance confidence.7 It has the potential to pre- dict future health status,8,9 and functional decline10 including hospitalization,11 discharge location,12,13 and mortality.14 Walk- ing speed reflects both functional and physiological changes,6 is a discriminating factor in determining potential for rehabili- tation,15 and aids in prediction of falls16 and fear of falling.17 Furthermore, progression of WS has been linked to clinical meaningful changes in quality of life18 and in home and com- munity walking behavior.19 Due to its ease of use20 and psycho- metric properties, WS has been used as a predictor and outcome measure across multiple diagnoses.8,9,19,21-26 In addition, WS was chosen by a panel of experts as the standardized assessment to measure locomotion for the Motor Function Domain of the NIH Toolbox.27
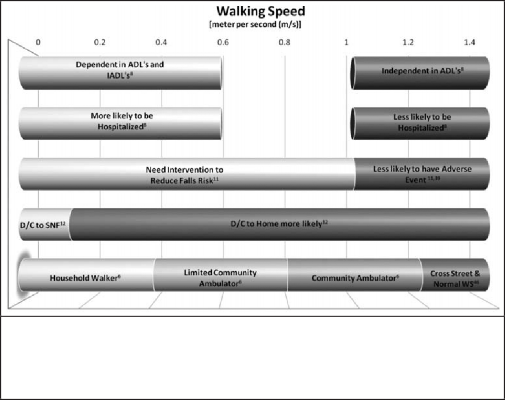
ADL: activities of daily living; IADL: instrumental ADLs; D/C: discharged; WS: walking speed; mph: miles per hour;
sec: seconds
Walking speed, like blood pres-
sure, may be a general indicator that can predict future events and reflect various underlying physi- ological processes.8 While WS can- not stand alone as the only predic- tor of functional abilities, just at blood pressure is not the only sign of heart disease; WS can be used as a functional “vital sign” to help determine outcomes such as func- tional status,6,8 discharge location,12 and the need for rehabilitation11 (Figure 1).
Downloaded from http://journals.lww.com/jgpt by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC1y0abggQZXdgGj2MwlZLeI= on 10/06/2021
| 0 mph | 0.4 mph | 0.9 mph | 1.3 mph | 1.8 mph | 2.2 mph | 2.7 mph | 3.1 mph |
| 10 meter walk time | 50 sec | 25 sec | 16.7 sec | 12.5 sec | 10 sec | 8.3 sec | 7.1 sec |
| 10 foot walk time | 15.2 sec | 7.6 sec | 5 sec | 3.8 sec | 3 sec | 2.5 sec | 2.2 sec |
Walking is a complex func- tional activity; thus, many vari- ables contribute to or influence WS. These include, but are not limited to, an individual’s health status,28 motor control,29 muscle performance and musculoskel- etal condition,30,31 sensory and perceptual function,32 endurance and habitual activity level,33 cog- nitive status,34 motivation and mental health,35,36 as well as the
formance measures used in conjunction with WS are often bet- ter able to predict health status,28 the use of WS alone can be an excellent predictor.11,20 For example, WS predicts the post hospital discharge location 78% of the time, and the addition of cognition or initial FIM scores does not significantly strengthen the ability of defining if a patient will be discharged to home or to a skilled nursing facility.12
Several standardized assessments and physical performance tests reliably predict function and health related events. Yet the consistent use of measures in physical therapy and other clinical settings is not widely practiced.38 Factors contributing to this non-use of standardized assessments may include insufficient time, inadequate equipment or space, or lack of knowledge in interpreting the assessment.39 Walking speed is one standard- ized measure that can be quickly and easily incorporated into the PT examination/evaluation process.
Determining feasibility is the first essential step in deciding to use a test or measure in the clinic. The main questions clini- cians should pose regarding a test’s or measure’s feasibility are:
- Is the test safe?
- Is it cost effective?
- How easy is the test to administer? and
- How easily are the results of the test graded and interpreted?characteristics of the environmentin which one walks.37 While per-Figure 1. A collection of walking speed times that are linked to dependence, hospitalization,rehabilitation needs, discharge locations, and ambulation category.An affirmative answer to all these questions, as there is with WS, lends to feasibility of use in a clinical setting. Walking speed is safe, requires no special equipment, adds no signifi- cant cost to an assessment, requires little additional time (can be administered in less than 2 minutes8), is easy to calculate (distance/time), and is easy to interpret based on published norms3,40-42
(Figure 2).
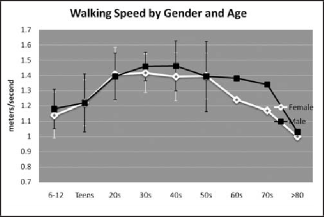
Figure 2. Self selected walking speed categorized by gender and age (6-12 and teens,47 20s-50s,42 & 60s-80s48).
Walking speed can be quickly and accurately assessed in the majority of physical therapy practice settings, including home care, subacute and acute rehabilitation facilities, long-term care facilities, out-patient offices, and schools, as well as during com- munity wellness/screening activities.43 Measurements of walk- ing speed are highly reliable, regardless of the method for mea- surement, for different patient populations and for individuals with known impairments affecting gait.3,42 Examination of WS requires a stopwatch and as little as a 20 foot space to walk forward.3 While most reported normative values are based on measuring in the middle two-thirds of a longer walkway, al- lowing walking speed to reach a steady state, others have used shorter distances.44,45 If possible, timing WS three times dur- ing the examination (with a few minutes of rest between trials) and developing a mean WS value will provide a more accurate estimate of actual self-selected walking speed than a single trial would.3,41,43Figure 3 displays a suggested reliable, inexpensive methodto collect WS by using the 10 meter (m) walk test.25 It re- quires a 20 m straight path, with 5 m for acceleration, 10 m for steady-state walking, and 5 m for deceleration. Markers are placed at the 5 and 15 m positions along the path. The patient begins to walk “at a comfortable pace”

at one end of the path, and continues walking until he or she reaches the other end. The Physical Therapist uses a stopwatch to determine how much time it takes for the patient to traverse the 10 m center of the path, starting the stopwatch as soon as the patient’s limb crosses the first marker and stop- ping the stopwatch as soon as the pa-If a full 20 m walkway is not available, shorter distances can be used, as long as there is adequate room for acceleration and deceleration (eg, 5 ft acceleration, 10 ft. steady state, 5 ft. de- celeration).While WS varies by age, gender, and anthropometrics, the range for normal WS is 1.2-1.4m/sec.46 This general guideline can help in monitoring our patients, along with norms by age 42,47,48(Figure 2), and other cited cutoff points6,8,11,12,46 (Figure 1). Interpretation of WS also includes understating what con- stitutes true change and what change may be due to measure- ment error.49 In a recent study, with a diverse group of older participants with varying diagnoses, 0.05 m/s was calculated as the needed change for a small but meaningful improvement in WS.25 In addition, for patients who do not have normal walk- ing speed, an improvement in WS of at least 0.1 m/s is a useful predictor for well-being,9,14 while a decrease in the same amount is linked with poorer health status, more disability, longer hos- pital stays, and increased medical costs.9 The MDC scores are specific to the population and will vary according to your cli- ent’s presentation.26,50Walking speed is an easily accessible screening tool11 that should be performed to offer insight into our patients function- al capacity and safety. Physical therapists, as specialists in move- ment and function, can use WS as a practical and informative functional sixth “vital sign” for all patients; examining walking speed in the same way that we routinely monitor blood pres- sure, pulse, respiration, temperature, and pain.51 This sixth “vi- tal sign” provides a relevant functional perspective to the health status provided by the system-level vital signs assessed on most visits to physicians’ offices.This review summarizes the strong psychometric properties of WS and robust evidence for using this clinical measurement. Walking speed is easily measurable, clinically interpretable,14 and a potentially modifiable risk factor.52 For these reasons, us- ing WS as the sixth vital sign is both pragmatic and essential.
REFERENCES- Wade D. Measurement in Neurological Rehabilitation. Ox-ford: University Press; 1992.
- Richards CL, Olney SJ. Hemiparetic gait following stroke. Part II: Recovery and physical therapy. Gait Posture. 1996:149-162.
- Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: Six- Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and gait speeds. Phys Ther. 2002;82:128-137.tient’s limb crosses the second marker. Figure 3. Suggested methods for collecting 10 meter walk test times.
- van Iersel MB, Munneke M, Esselink RA, Benraad CE, Olde Rikkert MG. Gait velocity and the Timed-Up-and- Go test were sensitive to changes in mobility in frail elderly patients. J Clin Epidemiol. 2008;61:186-191.
- Harada N, Chiu V, Damron-Rodriguez J, Fowler E, Siu A, Reuben DB. Screening for balance and mobility impair- ment in elderly individuals living in residential care facili- ties. Phys Ther. 1995;75:462-469.
- Perry J, Garrett M, Gronley JK, Mulroy SJ. Classifica- tion of walking handicap in the stroke population. Stroke. 1995;26:982-989.
- Mangione KK, Craik RL, Lopopolo R, Tomlinson JD, Brenneman S. Predictors of gait speed in patients after hip fracture. Physiother Can. 2007;59:10-18.
- Studenski S, Perera S, Wallace D, et al. Physical perfor- mance measures in the clinical setting. J Am Geriatr Soc. 2003;51:314-322.
- Purser JL, Weinberger M, Cohen HJ, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42:535-546.
- Brach JS, VanSwearingen JM, Newman AB, Kriska AM. Identifying early decline of physical function in commu- nity-dwelling older women: performance-based and self- report measures. Phys Ther. 2002;82:320-328.
- Montero-Odasso M, Schapira M, Soriano ER, Varela M, Ka- plan R, Camera LA, Mayorga LM. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60:1304-1309.
- Rabadi MH, Blau A. Admission ambulation velocity pre- dicts length of stay and discharge disposition following stroke in an acute rehabilitation hospital. Neurorehabil Neu- ral Repair. 2005;19:20-26.
- Salbach NM, Mayo NE, Higgins J, Ahmed S, Finch LE, Richards CL. Responsiveness and predictability of gait speed and other disability measures in acute stroke. Arch Phys Med Rehabil. 2001;82:1204-1212.
- Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better surviv- al in older adults. J Am Geriatr Soc. 2007;55:1727-1734.
- Goldie PA, Matyas TA, Evans OM. Deficit and change in gait velocity during rehabilitation after stroke. Arch Phys Med Rehabil. 1996;77:1074-1082.
- Guimaraes RM, Isaacs B. Characteristics of the gait in oldpeople who fall. Int Rehabil Med. 1980;2:177-180.
- Maki BE. Gait changes in older adults: predictors of falls orindicators of fear. J Am Geriatr Soc. 1997;45:313-320.
- Schmid A, Duncan PW, Studenski S, et al Improvements in speed-based gait classifications are meaningful. Stroke. 2007;38:2096-2100.
- Bowden MG, Balasubramanian CK, Behrman AL, Kautz SA. Validation of a speed-based classification system using quantitative measures of walking performance poststroke. Neurorehabil Neural Repair. 2008;22:672-675.
- Guralnik JM, Ferrucci L, Pieper CF, et al. Lower extrem- ity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221-231.
- Meyer-Heim A, Borggraefe I, Ammann-Reiffer C, et al. Feasibil- ity of robotic-assisted locomotor training in children with central gait impairment. Dev Med Child Neurol. 2007;49:900-906.
- Lee CE, Simmonds MJ, Etnyre BR, Morris GS. Influence of pain distribution on gait characteristics in patients with low back pain: part 1: vertical ground reaction force. Spine. 2007;32:1329-1336.
- Rochester L, Burn DJ, Woods G, Godwin J, Nieuwboer A. Does auditory rhythmical cueing improve gait in people with Parkinson’s disease and cognitive impairment? A Feasibil- ity study. Mov Disord. 2009. http://www3.interscience.wiley. com/journal/121685802/abstract
- Behrman AL, Lawless-Dixon AR, Davis SB, et al. Locomo- tor training progression and outcomes after incomplete spinal cord injury. Phys Ther. 2005;85:1356-1371.
- Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc. 2006;54:743-749.
- Palombaro KM, Craik RL, Mangione KK, Tomlinson JD. Determining meaningful changes in gait speed after hip frac- ture. Phys Ther. 2006;86:809-816.
- NIH Toolbox: Assessment of Neurological and Behavioral Function. Available at: www.nihtoolbox.org. Accessed March 12, 2009.
- Lord SE, Rochester L. Measurement of community ambu- lation after stroke: current status and future developments. Stroke. 2005;36:1457-1461.
- Gerin-Lajoie M, Richards CL, McFadyen BJ. The circumven- tion of obstacles during walking in different environmental contexts: a comparison between older and younger adults. Gait Posture. 2006;24:364-369.
- Buchner DM, Larson EB, Wagner EH, Koepsell TD, de La- teur BJ. Evidence for a non-linear relationship between leg strength and gait speed. Age Ageing. 1996;25:386-391.
- Ostchega Y, Dillon CF, Lindle R, Carroll M, Hurley BF. Isoki- netic leg muscle strength in older americans and its relation- ship to a standardized walk test: data from the national health and nutrition examination survey 1999-2000. J Am Geriatr Soc. 2004;52:977-982.
- teVelde A, Savelsbergh GJ, Barela JA, van der Kamp J. Safety in road crossing of children with cerebral palsy. Acta Paediatr. 2003;92:1197-1204.
- Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB. Characteristics of older pedestrians who have dif- ficulty crossing the street. Am J Public Health. 1997;87:393- 397.
- Persad CC, Jones JL, Ashton-Miller JA, Alexander NB, Gior- dani B. Executive function and gait in older adults with cogni- tive impairment. J Gerontol A Biol Sci Med Sci. 2008;63:1350- 1355.
- Lemke MR, Wendorff T, Mieth B, Buhl K, Linnemann M. Spatiotemporal gait patterns during over ground locomotion in major depression compared with healthy controls. J Psychi- atr Res. 2000;34:277-283.
- Fredman L, Hawkes WG, Black S, Bertrand RM, Magazin- er J. Elderly patients with hip fracture with positive affect have better functional recovery over 2 years. J Am Geriatr Soc. 2006;54:1074-1081.
- Robinett CS, Vondran MA. Functional ambulation veloc- ity and distance requirements in rural and urban communi- ties. A clinical report. Phys Ther. 1988;68:1371-1373.
- Duncan PW, Jorgensen HS, Wade DT. Outcome measures in acute stroke trials: a systematic review and some recommenda- tions to improve practice. Stroke. 2000;31:1429-1438.
- Cesari M, Kritchevsky SB, Penninx BW, et al. Prognosticvalue of usual gait speed in well-functioning older people–results from the Health, Aging and Body CompositionStudy. J Am Geriatr Soc. 2005;53:1675-1680.
- Oberg T, Karsznia A, Oberg K. Basic gait parameters: refer- ence data for normal subjects, 10-79 years of age. J Rehabil Res Dev. 1993;30:210-223.
- Lusardi M, Pellecchia G, Schulman M. Functional per- formance in community living older adults. J Geriatr Phys Ther. 2003;26:14-22.
- Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determi- nants. Age Ageing. 1997;26:15-19.
- Bohannon R. Measurement of gait speed of older adults is feasible and informative in a home-care setting. J Geriatr Phys Ther. 2009;32:22-23.
- Bohannon R. Population Representative Gait Speeds andits Determinants. J Geriatr Phys Ther. 2008;31:49-52.
- Centers for Disease Control and Prevention National Cen- ter for Health Statistics,National Health and Nutrition Ex- amination Survey Data. Hyattsville, MD: US Department of Health and Human Services, Centers for Disease Con- trol and Prevention, 2001-2002. Available at: http://www. cdc.gov/nchs/about/major/nhanes/nhanes01-02.htm. Ac- cessed March 12, 2009.
- Lerner-Frankiel M, Varcas S, Brown M, Krusel L, Schoneberger W. Functional community ambulation: what are your criteria? Clin Man Phys Ther. 1986;6:12-15.
- Waters RL, Lunsford BR, Perry J, Byrd R. Energy-speed relationship of walking: standard tables. J Orthop Res. 1988;6:215-222.
- Bohannon R. Comfortable Walking Speed: Norms for Adults derived Using Meta-Analysis. NIH Toolbox Confer- ence: Bethesda, MD. 2008.
- Hollman J, Becman B, Brandt R, Merriwether R. Mini- mum Detectable change in gait velocity during acute re- habilitation following hip fracture. J Geriatr Phys Ther. 2008;3:53-56.
- Fulk GD, Echternach JL. Test-retest reliability and minimal detectable change of gait speed in individuals undergoing re- habilitation after stroke. J Neurol Phys Ther. 2008;32:8-13.
- Guide to Physical Therapist Practice. Alexandria, Va: Amer- ican Physical Therapy Association; 2001.
- Dickstein R. Rehabilitation of gait speed after stroke: a crit- ical review of intervention approaches. Neurorehabil Neural Repair. 2008;22:649-660.





